
Knee pain is a common complaint in modern society. Knee pain can be debilitating, and a source for concern. In general, there are two types of patients with knee problems, younger more active individuals, and older patients with worn out joints. This difference lies in the type of conditions that arise.
Younger patients tend to have problems with tendons and ligaments within and around the knee. They tend to be more heavily involved in contact sports, so they might also suffer from injuries which may cause torn ligaments, cartilage/meniscus injuries and dislocated joints. Heavy involvement in sport may also result in overuse or strained/torn tendons.
Elderly patients generally accumulate small injuries to their knees throughout life. This accumulates in a condition known as osteoarthritis of the knee, in which the joint cartilage over the knee surfaces gets worn out. They frequently have pain with everyday motions, such as prolonged walking or standing, may have problems with stairs or slopes and may be unable to squat.
Pain can arise in the knee from several sources, damage to any of the above areas can result in pain in the knee. Most common, pain in the knee is felt in front or inside the knee (anterior knee pain). Sometimes, especially with meniscus injuries or muscle injuries, patients may feel pain at the back of the knee (posterior knee pain).
In the early stages of knee problems, knee pain usually happens with activity only (mechanical), but as the conditions worsen, patients may start to experience knee pain even without knee movement or activity.
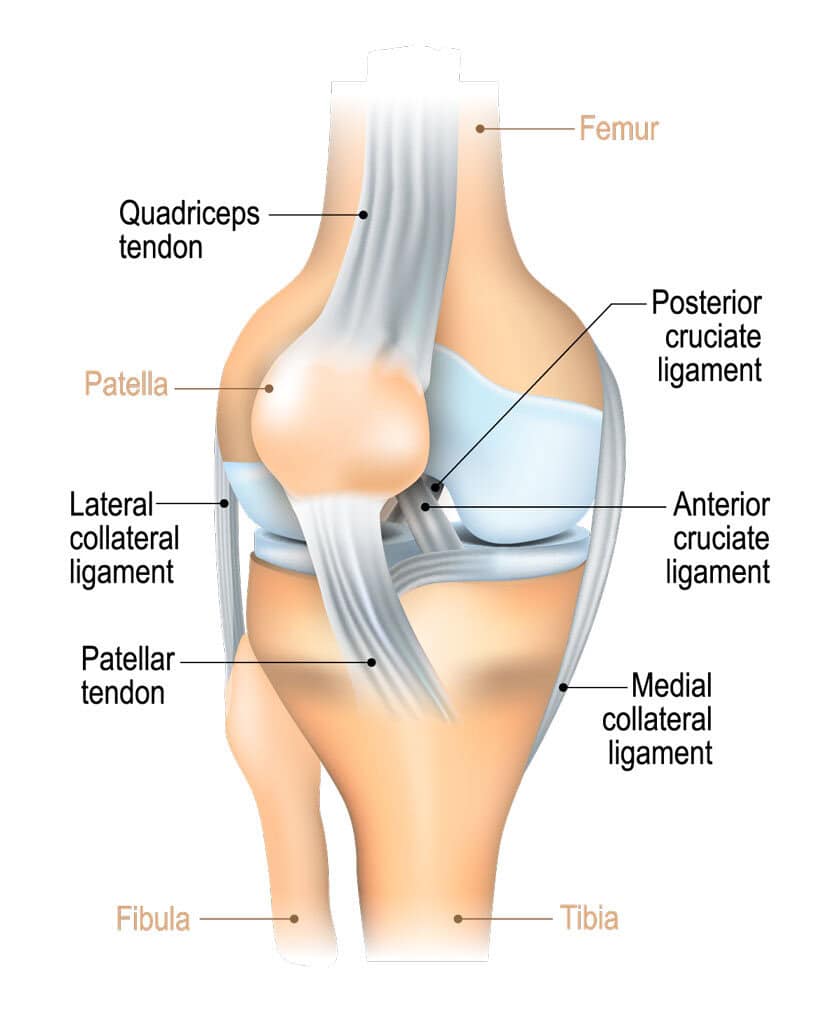
Parts of the knee which can cause pain include:
Knee pain can be associated with a variety of other symptoms, including:
As mentioned previously, knee pain in younger patients tends to arise due to injuries especially those sustained during sport. Patients will often give a history of a twisting injury to the knee, typically while standing on one leg only. Another common occurrence is for the injured knee to be hit from the side while the patient is standing.
A variety of injuries can result from these mechanisms:
Apart from injury, younger patients may also experience knee pain due to tendon overuse, which results in pain and swelling especially over the front of the knee. This most commonly affects the area above the kneecap, but can affect the area below it as well.
Age itself does not always mean that one will start to experience knee pain. However, age makes it more likely that your knee has sustained injuries throughout your life. As a result, older patients especially those above the age of 60 often suffer from worn out joints (knee osteoarthritis).
This is characterized by extensive loss of cartilage over the knee joint, and results in pain and stiffness. Many patients will find themselves losing knee function, and will have difficulty going up and down stairs. They usually also lose the ability to squat at an early stage, and learn mechanisms to cope.
Patients with knee pain will undergo a medical interview, and based on the information gained from the interview, patients will undergo a focused examination of the knee and the associated regions. This will provide the doctor with information pertaining to the underlying condition.
You may then be asked to undergo plain X-rays of the knee, and may also be asked to take standing X-rays of the leg to check leg alignment. In patients suspected of having ligament/meniscal damage, you may also be asked to go for an MRI scan.
Depending on the underlying condition, your treatment will be tailored for you. We provide a full suite of options to treat what ails you, be it surgical or non-surgical. In the knee these options include,
FAQs
Knee arthritis or more specifically knee osteoarthritis (OA), is the leading cause of knee pain in adults. It occurs when the cartilage that cushions your bones degrade over time. The cartilage may degrade through injuries or repetitive motions. The joint lining (synovium) inflames and results in knee pain, joint swelling, stiffness and difficulty walking. There may be creaking, clicking, grinding or snapping noises (crepitus), knee buckling, skin redness, locking of the knees, warm skin and joint pain that progresses slowly or pain that happens suddenly. The most common symptoms are pain and swelling of the knee joint. To properly diagnose oneself, please do seek professional help.
Non-surgical Options
Physical therapy
Physiotherapy is an essential part of non-surgical treatment of knee arthritis. Your physiotherapist may use heat treatments, range of motion exercises as well as targeted muscle strengthening to improve the function of your knee. While there is no evidence that this can help to slow down or reverse arthritis, it can lessen the symptoms of arthritis, and allow better knee function.
Lifestyle modifications
Having knee arthritis can impact many aspects of your life. Learning to cope with the changes brought about by this condition can help to alleviate symptoms, and can sometimes prevent injury.
Pain medication
Your doctor may prescribe pain medications such as non-steroidal anti-inflammatory drugs (NSAIDs), paracetamol (Acetaminophen/Tylenol/Panadol).
These medications can be used to alleviate most of the pain caused by knee arthritis, should be used judiciously due to possible side effects such as stomach ulcers and kidney damage for NSAIDs. Do not take more than the prescribed dosage and frequency, and inform the doctor if you feel unwell after taking such medications.
Knee Injections for the treatment of pain
Intra-Articular Hyaluronic Acid Injections, are injections filled with Hyaluronic Acid, that is injected into the joints. Hyaluronic Acid is a thick fluid. It is similar to the fluid in your body that naturally lubricates the joints. This helps patients feel less pain, improve mobility and reduce stiffness in joints. These results may last as long as 6 months. However, the specific ways of how it manages to do so are still unclear, and study results have been mixed about the effectiveness of this treatment.
Cortisone is a hormone that is naturally produced in your body, and is often used to reduce inflammation. It is effective for short-term pain relief in patients, however, Cortisone injections may worsen joint damage over time, so this option may not be suitable for all patients.
Autologous protein solutions (APS) injections are a newer category of knee injections that are derived from your own blood. This technique concentrates anti-inflammatory factors which are used to prevent inflammation in the knee. Current evidence suggests that inflammation in the knee is one of the factors that exacerbates the worsening of knee arthritis. Thus, it helps slow down the worsening of knee arthritis.
In most patients with knee arthritis, the body weight is carried on the inner portion of the knee joint. Consequently, most patients with knee arthritis suffer from medial (inner) compartment knee arthritis. Such patients would benefit from the shifting of their bodyweight, so that the weight is borne on the outer part of the knee instead. This can be achieved by a category of knee braces known as offloading braces. Depending on your specific needs, your surgeon may prescribe these braces as part of your treatment.
Surgical Options
Knee arthroscopy / Arthroscopic Surgery
Knee arthroscopy is a minimally-invasive surgical procedure. A small optic tube (arthroscope) with a light attached will be inserted into the joint through a small incision. Images of the inside of the joint are then projected onto a screen. Knee scopes help to assess changes caused by arthritis in the joint.
Subchondroplasty
Subchondroplasty is a relatively new procedure which was developed to treat pain in the knee arising from damage caused by OA to the bone of the shin or thigh bones. The loss of knee cartilage removes the protective effect of cartilage. As a result, patients often develop micro-fractures in the bone marrow/spongy bone of the shin or thigh bones. These so-called bone marrow lesions are partly responsible for the pain patients experience from knee OA. During the procedure, the affected area is drilled, and bone cement is injected into the lesion in order to treat it.
Subchondroplasty is beneficial because it helps patients reduce knee pain and improve their knee function, acting as a good alternative to joint replacement surgery. It is also minimally invasive (done with only small cuts and a few stitches), and patients are usually discharged on the same day as the surgery. This can lead to a faster recovery and quick return to normal activities. Lastly, if the patient needs to get total knee replacement in the future, Subchondroplasty will not hinder it as well.
If bone marrow lesions are the primary source of pain in your knee, this procedure may benefit you. However, this procedure may not work for everyone, so you should discuss this option with your Orthopaedic Surgeon before making a decision.
Knee realignment surgery
In this surgery, part of the shin or thigh bone is sawed and the alignment of your leg is changed in such a way as to remove pressure on the part of the knee that has arthritis changes. This helps to relieve some of the pain from the condition. This surgery helps as patients can avoid or delay going for a Total Knee Replacement Surgery.
It is not suitable for all patients, and a strict criterion is used to determine if you are suitable for such surgery. In general, patients who are younger (below 60 years old), lead active lifestyles, and only have arthritis in one area of their knee can consider this procedure.
After realignment surgery, the bones will be fixed with metal plates and screws, and these implants will maintain the realignment till the bone heals. This can take up to 6 months. During the recovery, you will be required to undergo regular physiotherapy treatments.
Partial knee replacement
In this procedure, your surgeon will only replace the most damaged portion of your knee with a metal and plastic partial knee prosthesis. This acts as an alternative to total knee replacement in patients who have knee arthritis in only some parts of the knee.
As this surgery is conducted through a smaller incision, and a smaller part of the knee is excised and replaced, the pain experienced is less than traditional total knee replacement. Patients heal faster, and generally have a quicker recovery period. It has also been shown that patients treated in this way have less complications compared to total knee replacement.
However, not all patients are suitable for this type of knee surgery. There is also a risk that the knee implants may wear out, or that significant knee arthritis can develop in other parts of the knee, necessitating subsequent total knee replacement surgery (10 to 12 years).
Total knee replacement
This is a procedure where your surgeon will cut away damaged bone and cartilage from your thigh bone, shinbone and kneecap, replacing it with a prosthetic joint made of metal alloys, high-grade plastics and polymers. This is the gold standard treatment for late-stage knee OA.
The procedure takes about 2 hours, and rehabilitation and recovery from surgery can take 3 to 6 months. In general, most patients find themselves walking unaided after 6 weeks post-surgery. The knee prosthesis that is inserted in this way is long-lasting and sturdy, with implants surviving up to 25 years in some international studies.
Because of implant survivorship, it is recommended that only patients above the age of 60 undergo this procedure. This surgery is sometimes offered to younger patients especially if they already have end stage knee arthritis.
Knee osteoarthritis (OA) is the leading cause of knee pain in adults, with roughly 250 million people affected by it worldwide .
It occurs when the smooth and thin lubricating layer which covers the ends of bones (also known as articular cartilage) wears away. The degradation of this cushioning cartilage reduces the shock absorbing benefits available, causing the joint lining at the knee to be inflamed. In severe cases of knee osteoarthritis, the bones may rub directly against each other causing great pain and disability.
Additionally, knee osteoarthritis can also result in the formation of bone spurs, smooth hard bumps of extra bone at the joints, which can cause pain if they press against nerves.
How is osteoarthritis of the knee treated?
Non-surgical Options
Physical therapy
Physiotherapy is an essential part of non-surgical treatment of osteoarthritis. Your physiotherapist may use heat treatments, range of motion exercises as well as targeted muscle strengthening to improve the function of your knee. While there is no evidence that this can help to slow down or reverse osteoarthritis, it can lessen the symptoms of osteoarthritis, and allow better knee function.
Lifestyle modifications
Osteoarthritis can impact many aspects of your life. Learning to cope with the changes brought about by osteoarthritis can help to alleviate symptoms, and can sometimes prevent injury. Modifications in your lifestyle are hence an important part of osteoarthritis treatment.
These can include,
Pain medication
Your doctor may prescribe pain medications such as non-steroidal anti-inflammatory drugs (NSAIDs), paracetamol (Acetaminophen/Tylenol/Panadol).
These medications can be used to alleviate most of the pain caused by osteoarthritis, but should be used judiciously due to possible side effects such as stomach ulcers and kidney damage for NSAIDs. Do not take more than the prescribed dosage and frequency, and inform the doctor if you feel unwell after taking such medications.
If you find yourself relying too much on such medication, consider other forms of treatment, as pain medications alone cannot heal your knee, and may not be sufficient to control your pain.
Oral supplements
There are a variety of oral supplements available for the treatment of osteoarthritis. Unfortunately, there is currently no evidence that shows that taking any oral supplements can heal knees affected by osteoarthritis. Some patients may however find that their knee pain is slightly relieved after taking these supplements. Most of such supplements are safer than traditional pain medication, and your doctor may suggest that you try these supplements to see if it helps in relieving your knee pain.
Knee Injections for the treatment of pain
Intra-Articular Hyaluronic Acid Injections, are injections filled with Hyaluronic Acid, that is injected into the joints.
Hyaluronic Acid is a thick fluid. It is similar to the fluid in your body that naturally lubricates the joints.
This helps patients feel less pain, improve mobility and reduce stiffness in joints. These results may last as long as 6 months.
However, the specific ways of how it manages to do so are still unclear, and study results have been mixed about the effectiveness of this treatment.
Cortisone is a hormone that is naturally produced in your body, and is often used to reduce inflammation.
It is effective for short-term pain relief in Osteoarthritis patients, however, Cortisone injections may worsen joint damage over time, so this option may not be suitable for all patients.
Autologous protein solutions (APS) injections are a newer category of knee injections that are derived from your own blood. This technique concentrates anti-inflammatory factors which are used to prevent inflammation in the knee. Current evidence suggests that inflammation in the knee is one of the factors that exacerbates the worsening of knee OA. The benefit therefore of injecting APS solutions into the knee is that it may slow down the development of more severe knee OA.
In most patients with knee OA, the body weight is carried on the inner portion of the knee joint. Consequently, most patients with knee OA suffer from medial (inner) compartment knee OA. Such patients would benefit from the shifting of their bodyweight, so that the weight is borne on the outer part of the knee instead. This can be achieved by a category of knee braces known as offloading braces. Depending on your specific needs, your surgeon may prescribe these braces as part of your treatment.
Surgical Options
Knee arthroscopy / Arthroscopic Surgery
Knee arthroscopy is a minimally-invasive surgical procedure. A small optic tube (arthroscope) with a light attached will be inserted into the joint through a small incision. Images of the inside of the joint are then projected onto a screen. Knee scopes help to assess changes caused by arthritis in the joint. In early knee OA, knee scopes can be used to treat menisceal tears and small holes in the cartilage. This procedure may be suitable for your stage of knee OA. Please seek help from your surgeon to determine if this is the surgery for you.
Subchondroplasty
Subchondroplasty is a relatively new procedure which was developed to treat pain in the knee arising from damage caused by OA to the bone of the shin or thigh bones. The loss of knee cartilage removes the protective effect of cartilage. As a result, patients often develop micro-fractures in the bone marrow/spongy bone of the shin or thigh bones. These so-called bone marrow lesions are partly responsible for the pain patients experience from knee OA. During the procedure, the affected area is drilled, and bone cement is injected into the lesion in order to treat it.
Subchondroplasty is beneficial because it helps patients reduce knee pain and improve their knee function, acting as a good alternative to joint replacement surgery. It is also minimally invasive (done with only small cuts and a few stitches), and patients are usually discharged on the same day as the surgery. This can lead to a faster recovery and quick return to normal activities. Lastly, if the patient needs to get total knee replacement in the future, Subchondroplasty will not hinder it as well.
If bone marrow lesions are the primary source of pain in your knee, this procedure may benefit you. However, this procedure may not work for everyone, so you should discuss this option with your Orthopaedic Surgeon before making a decision.
Knee realignment surgery
In this surgery, part of the shin or thigh bone is sawed and the alignment of your leg is changed in such a way as to remove pressure on the part of the knee that has OA changes. This helps to relieve some of the pain from Osteoarthritis. This surgery helps as patients can avoid or delay going for a Total Knee Replacement Surgery.
It is not suitable for all patients, and a strict criteria is used to determine if you are suitable for such surgery. In general, patients who are younger (below 60 years old), lead active lifestyles, and only have OA in one area of their knee can consider this procedure.
After realignment surgery, the bones will be fixed with metal plates and screws, and these implants will maintain the realignment till the bone heals. This can take up to 6 months. During the recovery, you will be required to undergo regular physiotherapy treatments.
Partial knee replacement
In this procedure, your surgeon will only replace the most damaged portion of your knee with a metal and plastic partial knee prosthesis. This acts as an alternative to total knee replacement in patients who have knee OA in only some parts of the knee.
As this surgery is conducted through a smaller incision, and a smaller part of the knee is excised and replaced, the pain experienced is less than traditional total knee replacement. Patients heal faster, and generally experience quicker recovery after partial knee replacement. It has also been shown that patients treated in this way have less complications compared to total knee replacement.
However, not all patients are suitable for this type of knee surgery. There is also a risk that the knee implants may wear out, or that significant knee OA can develop in other parts of the knee, necessitating subsequent total knee replacement surgery (10 to 12 years).
Total knee replacement
This is a procedure where your surgeon will cut away damaged bone and cartilage from your thigh bone, shinbone and kneecap, replacing it with a prosthetic joint made of metal alloys, high-grade plastics and polymers. This is the gold standard treatment for late-stage knee OA.
The procedure takes about 2 hours, and rehabilitation and recovery from surgery can take 3 to 6 months. In general, most patients find themselves walking unaided after 6 weeks post-surgery. The knee prosthesis that is inserted in this way is long-lasting and sturdy, with implants surviving up to 25 years in some international studies.
Because of implant survivorship, it is recommended that only patients above the age of 60 undergo this procedure. This surgery is sometimes offered to younger patients especially if they already have end stage knee OA.
Yes, pain in the back of the knee could be due to arthritis. Arthritis, or more specifically, Osteoarthritis, is a condition that wears down the cartilage of the joints over time. This condition can easily cause pain in the back of the knee. Patients with this condition in the knee may experience other symptoms such as joint swelling, stiffness and difficulty walking. Inflammation in the joint may make it stiff and painful. A person may also feel this discomfort in other areas around the knee joint. Other forms of arthritis that could be causing the pain include autoimmune conditions such as lupus and rheumatoid arthritis.
Walking is a good way to exercise with arthritis. It is an activity one can do even with stiff or sore knees. It can help ease joint pain, strengthen the leg muscles, improve one’s posture and improve one’s flexibility. It is also good for your heart. Remember to start slow and be careful of how your knee feels after walking. Patients with arthritis can also partake in low-impact activities. These are exercises that are easy on the knees such as swimming, cycling or other water sports. Water exercises takes the weight of the painful joints which minimizes the impact of the action on the knees. Being active would additionally help patients to lose weight which further takes pressure off the joints. Please ask your doctor or physical therapist on advice on what activities one should do.
The most common cause of swollen and painful knees is the condition, Arthritis. Arthritis is a broad term that refers to swelling and tenderness of one or more joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. The most common types of arthritis is osteoarthritis. Autoimmune conditions can also affect joints, such as rheumatoid arthritis. Metabolic conditions, such as gout can also cause other forms of arthritis. These conditions damage the joints and ultimately also lead to osteoarthritis.
Yes, there can be many causes of knee pain besides swelling. The most common causes of knee pain are related to aging, injuries or repeated stress on the knee. Common knee problems include sprained or strained ligaments, cartilage tears, tendonitis, and arthritis. For many of these conditions, the cause of the pain is not swelling but more of the symptom because of other problems in the knee joint. For example, for osteoarthritis which is the disease where there is a breakdown of the cushioning cartilage in the knee the pain is mainly due to the bones rubbing each other. As a result of that rubbing, it causes the knee to swell.
There are many treatments available for a swollen and painful knee dependent on the severity of the pain and the diagnosis given by the doctor. There are both non-surgical and surgical options for treatment. For less severe knee cases and for those who are not keen to go under the knife, physiotherapy and injections are an option. However, these treatments only provide a temporary solution and there is a limit to their effect in alleviating the pain and symptoms of the condition. In order to fix the underlying problem of the knee pain, surgery may be required. Such knee surgeries are partial knee replacement, knee replacement or subchondroplasty.
For swelling and pain in the knee a cold compress could be used to reduce the swelling. For a more long-term non-surgical remedy, physiotherapy or wearing a knee brace is recommended. Physiotherapy will help strengthen the muscles around the knee to reduce the stress on the joint. Wearing a knee brace will also help strengthen the joint and provide support. One should still consult a doctor before employing any natural remedy. Do take note that these remedies may or may not work and its effects are limited. More interventional solutions such as surgery may have to be considered for conditions to improve.
No, having trouble bending one’s knee is not normal as there is an underlying issue that is hindering the knee’s full motion. Pain is the body’s way of preventing you from making an injury worse. Since pain may limit movement, it can cause stiffness in the knees. There may also be swelling in the knee due to the build up of excess fluids in the joints caused by overuse, injury and medical condition. This can cause the sensation of tightness along with pain. The swelling may not be obvious so one might feel it as the stiffness of the knee. Swelling in the knee will limit motion. Pain and swelling are two preventive measures the body uses but also together they can lead to stiffness in your knee.
The most common cause of knee pain is Arthritis. Arthritis is the swelling and tenderness of one or more joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. Arthritis is the broad term, and the most common types of arthritis are osteoarthritis and rheumatoid arthritis. Most types of arthritis have be said to be caused by a problem in the immune system where the body starts to attack its own tissues in the joints. This may be inherited genetically. Other forms of arthritis can be caused by a metabolic condition, such as gout.
The pain from knee conditions, although painful, are often bearable. These symptoms are not associated with life-or-death diseases. Most patients can continue with daily activity although the intensity of the activity may have to decrease. However, the fact they can continue with day-to-day living makes seeking professional help seem unnecessary and they may not see the urgency in getting treated. Many patients are uninformed about the true realities of knee health and thus, they are unaware of the potential that their condition can worsen if not treated early. These patients then only seek help when their knee pain has gotten worse and to the point where their standard of living is significantly affected.
Non-surgical treatment for knee pain include:
Physical therapy
Your physiotherapist may use heat treatments, range of motion exercises as well as targeted muscle strengthening to improve the function of your knee. While there is no evidence that this can help to slow down or reverse the underlying knee condition that is causing the pain, it can lessen the pain, and allow better knee function.
Lifestyle modifications
Modifications in your lifestyle are important to prevent further injury and even lessen the pain.
These can include,
Pain medication
Your doctor may prescribe pain medications such as non-steroidal anti-inflammatory drugs (NSAIDs), paracetamol (Acetaminophen/Tylenol/Panadol).
Oral supplements
Some patients may however find that their knee pain is slightly relieved after taking these supplements. Most of such supplements are safer than traditional pain medication, and your doctor may suggest that you try these supplements to see if it helps in relieving your knee pain.
Knee Injections for the treatment of pain
Intra-Articular Hyaluronic Acid Injections, are injections of Hyaluronic Acid, that are injected into the joints. Hyaluronic Acid is a thick fluid. It is similar to the fluid in your body that naturally lubricates the joints. This helps patients feel less pain, improve mobility and reduce stiffness in joints. These results may last as long as 6 months. However, the specific ways of how it manages to do so are still unclear, and study results have been mixed about the effectiveness of this treatment.
There is always risk that comes with surgery. However, these complications are rare. First would be undergoing anaesthesia. Anaesthesia is very safe but has side effects such as sickness and confusion. There is a mild risk of more serious complications. Before going to surgery, your anaesthetist will explain the risks to you. Post-surgery, patients may be at risk to: