What are proximal femur fractures?
Proximal femur fractures are fractures that occur within the hip region. They mainly occur in older patients, especially those with osteoporosis, but can also occur in younger patients due to high-impact trauma.

The femur is the hip bone that links the knee joint to the hip joint. The proximal femur would hence be the part of the femur which is closer to the hip joint. It includes the femoral head and neck, amongst other regions.
What is the purpose of the femur bone?
The femur bone is very important. It helps to stabilise your movement when you walk and also is necessary to spread out your body weight.
There are a few main types of hip fractures: femoral neck fractures, femoral head fractures, intertrochanteric fractures, and subtrochanteric fractures.
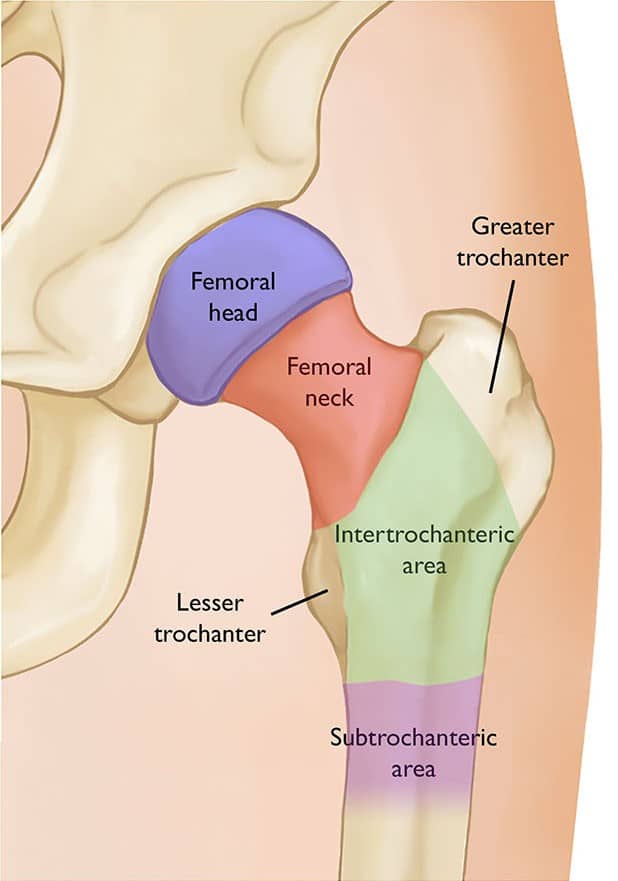
Femoral neck fractures are the most common location of hip fractures, accounting for around 50% of such fractures. Some femoral neck fractures are considered intracapsular, which means that the fracture is within the hip joint. This distinction is important because intracapsular fractures can cut off the blood supply to the bone of the femoral head, which may lead to bone death, a condition known as avascular necrosis (AVN).
Intertrochanteric fractures occur a little less frequently than femoral neck fractures. They are also fractures of the femur and are located outside the fibrous joint capsule. These fractures happen more commonly in elderly patients.
Subtrochanteric fractures are the least common type of hip fracture, accounting for 5-15% of all hip fractures, and are also the most difficult to fix as they are the least stable.
What are the causes of proximal femur fractures?
Older patients typically have such fractures due to low-impact trauma.
Low-impact trauma includes
The elderly are more susceptible to hip fractures as they are more likely to have low bone mass, where the bones become weaker and brittle. They are likely to have vision or balance problems, which increases the risk of them suffering a particularly bad fall that can cause a hip fracture.
High-impact trauma includes
What are the signs and symptoms of proximal femur fractures?
There are various signs and symptoms for a proximal femur fracture and vary based on the individual and the severity of the injury. However, common symptoms include
How are proximal femur fractures diagnosed?
The doctor will conduct a medical interview during which he/she will ask about the pain and the cause of the injury. He/she will also ask about your pre-existing medical conditions, such as osteoporosis.
He/she will then perform a focused examination on the injured hip, paying attention to any open wounds, and the circulation and nerves of the leg affected.
Following this examination, you will be asked to undergo x-rays of the hip and pelvis, to confirm the diagnosis of a hip fracture. Occasionally, additional x-rays, CT, or MRI scans may also be necessary especially if the fracture is not well visualised on x-rays.
What is the treatment like for proximal femur fractures?
Treatment options vary based on the age and activity level of the patient, as well as the severity of the injury, amongst other factors that may influence the chances of a successful recovery following surgery.
In most cases of proximal femur fracture, surgery is advised, as the immobility caused by these fractures can have severe effects on the patient. Immobile patients are more prone to chest and urinary infections may develop blood clots in the leg veins and may develop pressure ulcers from prolonged bed rest. In general, complications arising from an unoperated proximal femur fracture have been implicated as the cause of death in up to 25% of patients in the first year after the fracture.
Surgical options include,
AVN leads to the collapse of the femoral head bone, which will cause even more pain and immobility to the patient. If there is a risk of AVN, your doctor will strongly encourage partial hip replacement rather than hip fixation.
What is the rehabilitation process like?
After surgery, the physical therapist will likely guide the patient on mobilisation, so that the patient can begin to restore their hip function and preserve their range of motion. The patient will learn how to use mobility aids, which may be beneficial or necessary after the surgery, especially if the patient is older and has balance or vision problems that may increase the risk of a repeat fall after recovery.
The patient will be taught strengthening exercises so that they can gain function of their hip back and hopefully return to normal physical activity that they were involved in prior to the accident.
Most people take around 10-12 weeks to get close to full recovery, but it may be a year post-injury for the patient to fully recover.
For an assessment of your condition, please book an appointment with Dr. Yong Ren.